An emotional call to action: reclaim work–life balance with tools built for your reality.
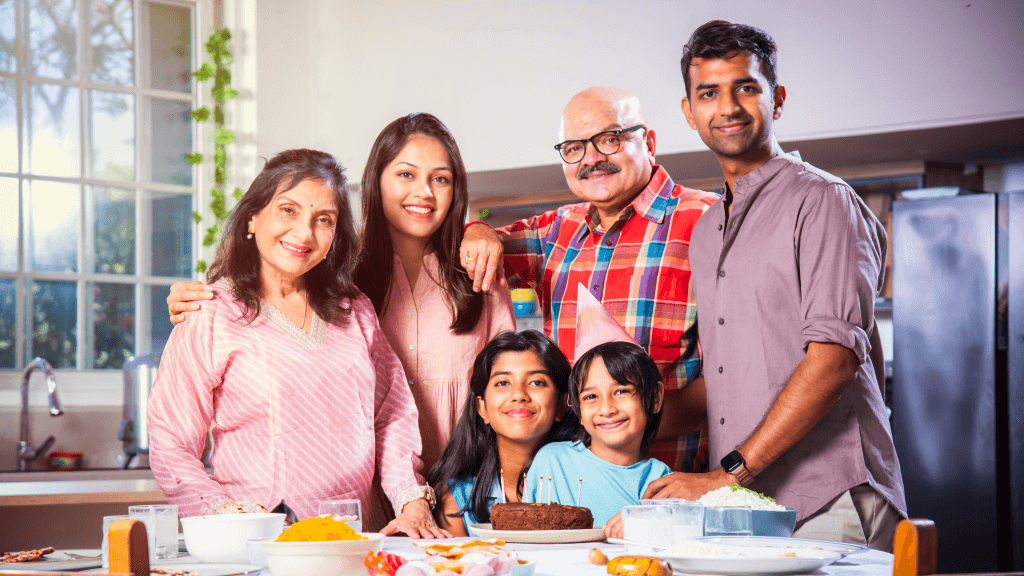
The missed dinner
It’s 7:45 p.m. again. Someone at home texts, “Khana garam kar doon?” You reply, “Bas 20 minutes.” You mean it—every time. But the OPD ran long, a parent wanted last visit notes, billing had a mismatch, and the pharmacy called twice about brands. By the time you leave, dinner is a reheat and your mind is still at the clinic.
You don’t need to work more. You need your time back.
The promise you made
You chose medicine to heal, not to wrestle with files, tabs, and tally sheets. Your value is clinical judgement, counselling, and continuity—not retyping the same advice or chasing missing bills. This is about dignity, family, and the kind of care only a rested doctor can give.
Where your evenings disappear
It’s rarely one big thing. It’s a hundred small ones.
- Repetition: Writing similar prescriptions and advice blocks again and again.
- Hunting: “Last time kya likha tha?” turns into a file search during consultation.
- Tab-hopping: EMR → billing → pharmacy → lab → back to EMR.
- No-shows & surprises: Weak reminders, last-minute stockouts.
- Day-close stress: Cash/UPI mismatch, missed add-ons, manual reconciliation.
A few “lost” minutes per patient becomes an hour—every day.
The human cost
Those minutes are stolen from your consult presence and your home. Decision fatigue creeps in; counselling gets rushed. Staff feel the strain; family hears another “kal pakka.” Burnout isn’t just hard on you—it shows up in the quality of care and patient trust.
What changes when the tools fit your flow
When your system thinks like a doctor, minutes return quietly to your day.
- One-screen consult: Notes, history, orders, and billing in one view—no tab tango.
- Templates & peek view: Common cases in a tap; last visit, allergies, and active meds visible instantly.
- Single-point entry: Update once; pharmacy, lab, and billing auto-sync.
- Missed-charge prompts & rate control: Fewer “adjust kar dena” moments, fewer desk delays.
- Automated reminders: Reduce no-shows; queue becomes predictable.
- Day-close reconciliation: Cash/UPI/cards tallied in minutes; variance flagged the same day.
Minutes saved per consult add up to evenings that end on time.
Three short stories from real clinics
Solo GP: Reused prescription templates for common complaints; stopped retyping long advice. She now finishes on time three days a week—without seeing fewer patients.
“Same cheezein baar-baar likhna band ho gaya.”
Pediatric clinic: As consult ends, invoice is already synced; parents don’t wait at the desk.
“By the time they reach billing, the bill is ready.”
Two-doctor OPD: WhatsApp/SMS reminders cut no-shows by a third; the queue finally flows.
“Files nahi dhoondni padti—context milta hai turant.”
A one-week reset you can start now
- Save top-10 templates & advice blocks for your most common conditions.
- Link Rx → billing → pharmacy; enable prompts for consumables/procedures.
- Turn on follow-up reminders (WhatsApp/SMS) to protect high-value slots.
- Run a 10-minute day-close checklist daily; reconcile cash/UPI/cards.
- Review anomalies weekly; tweak only 2–3 rules at a time.
You’ll feel the difference in seven days.
Objections, gently answered
- “Will it be hard to learn?” If you can use WhatsApp, you can use a doctor-designed system.
- “Do I need servers or IT?” No—go live without hardware headaches.
- “What about old data?” Patient master and prescriptions can be imported safely.
- “Will my staff manage?” Guided onboarding for reception, nursing, pharmacy—role-based views keep things simple.
Dinner, not dashboards
You deserve to be home for dinner—and to be fully present when you get there. Balance doesn’t come from longer hours. It comes from fewer frictions between you and your next clinical decision.
Try a one-screen, doctor-designed workflow and finish on time—starting next week.